(Editor’s Note: Jill Smith is a name given to an Oklahoma City resident who was interviewed about her mental health issues for this story.)
Jill Smith ran headlong into the unfairness surrounding mental health insurance in 2007. Her depression turned suicidal. In the grip of despair, she reached out to a friend for help and found herself at Oklahoma City’s Valley Hope. A social worker there referred her to an inpatient psychiatric hospital in Texas.
Counselors at the hospital recommended a 30-day stay. Desperate for help, Smith took them up on it. She had every reason to believe her stay would be covered by her private insurance plan. The plan did cover mental health services if they were a “medical necessity.” To her, the treatment wasn’t just a necessity — it was the difference between life and death.
But five days into her stay, Smith received devastating news. Her plan would not cover her treatment, deeming it “unnecessary.” The decision likely would have been different if Smith had presented with diabetes or a heart condition. Family members and friends banded together to cover the cost.
“When insurance didn’t pay, and then when the crisis hit again, it was the most hopeless and helpless feeling,” Smith said. “Plus, I knew it was causing financial stress for loved ones, which I had and have a huge amount of guilt for. It was disappointing and embarrassing as well.”
Despite federal mental health parity laws enacted in 2008, stories like Smith’s are still common, even being investigated in detail by 60 Minutes in 2014.
Today, Smith is insured by Insure Oklahoma, Oklahoma’s premium-assistance insurance plan for low-income workers who net too much money to be eligible for SoonerCare but not enough money to purchase plans through the Affordable Care Act’s federal exchange. Insure Oklahoma offers fairly comprehensive mental health coverage, but Smith said she is limited to only those providers that have contracted with the agency to deliver services.
How insurance agencies, public and private, interpret “parity” determines whether millions of Americans — and hundreds of thousands of Oklahomans — can receive much-needed mental health care. In some cases like Smith’s, lives hang in the balance. Oklahoma has one of the highest suicide rates in the nation.
“Getting mental health parity passed was a pivotal moment in eventually making Oklahoma health insurance plans provide equal coverage for mental and physical health care,” said Mike Brose, the executive director of Mental Health Association Oklahoma, a Tulsa nonprofit dedicated to the state’s mental wellness. “However, the letter of the law isn’t enough. There are many loopholes and exemptions from coverage, forcing many Oklahomans to go without treatment. There is still much work to be done to ensure that access to care exists so all Oklahomans impacted by mental illness can overcome the barriers to quality, appropriate care.”
The National Alliance on Mental Illness (NAMI) describes parity concisely:
When a plan has parity, it means that if you are provided unlimited doctor visits for a chronic condition like diabetes then they must offer unlimited visits for a mental health condition such as depression or schizophrenia.
A lot of ink has been used chronicling the plight of impoverished and uninsured mental health patients. But without mental health parity, even the insured won’t have access to needed mental health services, Brose said. That’s especially troubling in Oklahoma, where roughly 600,000 residents report having a mental illness, according to Mental Health America.
Oklahoma ranks second in the nation in per capita incidences of mental illness, according to the Substance Abuse and Mental Health Services Administration.
“Oklahoma has among the highest rates of mental illness and substance-abuse issues in the country, yet the majority of Oklahomans in need of treatment do not get the services they need to find recovery,” said Terri White, commissioner of the Oklahoma Mental Health and Substance Abuse Services (ODMHSAS) department. “There are too few resources in the public system to keep up with demand. But, what surprises many, is that even Oklahomans who have health insurance experience difficulty finding appropriate care.”
Who’s on board?
The good news is that SoonerCare, the largest insurer in Oklahoma, is mandated to offer mental health parity. The bad news is that state funding for mental health care is being cut, and service options are being limited.
RELATED
“Proposed rule would deny kids mental health access” by Aaron Askew
Insurers offering plans through the federal marketplace exchanges are also mandated to offer mental health parity. But Medicare isn’t subject to the same laws. Neither are most private plans, even when offered by an employer.
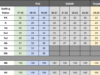
The number of Oklahomans seeking coverage with ACA plans jumped this year, jumping from 126,115 in 2015 to 145,329.
The federal government requires employers with 51 or more employees to cover mental health on par with other medical benefits — but only if the plans cover mental health at all. Mental health coverage is not mandatory. Companies too small to fall under the aegis of federal parity laws comprise well above 20 percent of businesses in Oklahoma.
Further compounding the problem, Gov. Mary Fallin declined Medicaid expansion offered by the ACA. That left about 100,000 Oklahomans — roughly one-sixth of Oklahomans struggling with mental illness — to fall into what’s become known as the “coverage gap,” according to the Kaiser Family Foundation. Another way of looking at that figure: Medicaid expansion would cover 80 percent of people with no insurance in the state’s mental health programs, according to Oklahoma Watch.
But things might get worse for SoonerCare clients. The state’s budget shortfall threatens many of the mentally ill insured by Medicaid. ODMHSAS may remove many of them from the state-sponsored insurance program, since the agency needs to absorb about $9.8 million in budget cuts. The state recently announced that the budget shortfall is larger than originally predicted, and deeper cuts in all state agencies will be needed.
The real world
Even when a plan is mandated to offer parity, the real world rears its ugly head. The insured still face roadblocks on the way to mental health recovery. Parity on paper doesn’t translate to real-world parity.
Mental health providers aren’t required to accept SoonerCare. They’re not required to accept any health insurance at all, and many don’t. That further strangles a mental health system already suffering from a lack of providers.
It’s also the reason that Oklahoma psychiatrists earn roughly $216,000 per year, according to U.S. News & World Report. They are among the top-10 earners in their field across the nation. When demand is high and supply is low, there’s no incentive for providers to accept certain insurances. Clients in need of care will, and do, pay out of pocket. And they’re charged top dollar. But for many, those costs are prohibitive. Mental health care is a pipe dream for them.
Lackluster enforcement of mental health parity laws also leave many out in the cold.
“Individuals with brain disease do not have the same access to care as is available for other illnesses. That must change. Brain health is imperative to overall health, and it is the biggest public health concern for our state, affecting one in four Oklahomans,” said White.
Location, location, location
There are only 571 licensed psychologists in the state, making for a ratio of one therapist for every 1,051 Oklahomans in need. The numbers are similar for psychiatrists.
They’re especially bleak in rural areas, of which the state has plenty. SAMSHA estimates that 55 percent of counties in the nation are without any mental health providers. For many seeking help for mental illness, it can be quite a haul. Elk City epitomizes the issue.
Even if the haul isn’t that long, rural psychiatrists charge more than their counterparts in urban areas.
You get what you pay for
SoonerCare only reimburses mental health care providers at, on average, 72 percent of the cost of their services, according to ODMHSAS in a recent budget proposal. This severely erodes the incentive of providers to accept SoonerCare. Add in the administrative hassles and paperwork that come with Medicaid, and many private, solo practitioners will not accept it.
Accepting SoonerCare can add an additional and costly level of bureaucracy for providers.
“It probably would take at least a part-time billing person. That’s the way most agencies do it if they really do a lot of Medicaid and Medicare,” said John Goetz, the clinical director for Edmond Family Counseling. “In their office, they have someone who does those claims and they’re very familiar with the process and how you fill out the information, checking the appropriate boxes, etc.”
Provider-reimbursement rates vary across private insurance plans, but they, too, typically reimburse mental health care providers at a lower rate. This leaves patients with higher out-of-pocket costs in the form of high deductibles and co-pays. In an effort to save money, many insured by the ACA often select plans with high out-of-pocket costs — large deductibles and co-pays. These costs, as well, can stymie many Oklahomans’ efforts to pursue mental health care.
The paper mountain
NAMI also notes that insurance companies often inject significant administrative obstacles to obtaining mental health care in their policies. In other words, the mountain of approvals and paperwork is too high for many to climb — for providers and patients.
A bronze-level ACA plan offered by Blue Cross Blue Shield of Oklahoma requires preauthorization for just about every potential mental health service. It can be a lengthy process, and often not one that users have time to undertake if a crisis hits. Failure to preauthorize results in a $500 fine. The same preauthorization is often not required for garden-variety medical services, though it largely affects medications.
Jumping through administrative hoops is no guarantee that insurers will authorize treatment. NAMI estimates that mental health services are denied by insurers in one-third of patients’ searches for mental health care.
The loophole employed by insurance companies in these instances is the lack of a clear definition of “medical necessity.” Without transparency, insurers can slip the chains of parity arbitrarily.
When patients are arbitrarily denied care, many of them roll into the public mental health care system. This costs taxpayers money that insurance companies would otherwise be doling out.
Getting into the weeds
Marketplace plans and private plans are often murky when it comes to disclosing mental health benefits. It’s a problem that probably plagues many private plans, too. It erodes real-world parity by leaving consumers with cost as the only decision rule.
All ACA plans, for example, are required to post a summary of benefits on the federal exchange, but these summaries are exactly that: short, truncated lists of benefits. They frequently lack specificity.
Again, NAMI explains:
These documents do not include the kind of detailed information about coverage that mental health consumers need to make informed decisions about the plans that are best for them.
This is typically true of every insurance plan, whether parity is present or not. Even documentation about how to write a summary of benefits can be murky. Detailed lists of benefits often run more than 100 pages and are mired in legalese.
All of this translates into a high number of untreated mentally ill adult Oklahomans — 66 percent, according to Mental Health America.
The stakes in Oklahoma’s mental health care game are high. The untreated mentally ill negatively affect families, communities and workplaces. But until the state achieves true, real-world parity, tens of thousands of what White terms “walking wounded” will pay the price.
“These illnesses can be successfully treated, especially when we get people needed help early in the disease process. Left untreated, mental illness and addiction lead to negative consequences for the individual, families, communities and our state as a whole. Access to appropriate care saves lives. We need to fix disparities in the system,” she said.
(Disclosure: NonDoc editor in chief William W. Savage III is a nationally certified Mental Health First Aid instructor who occasionally contracts with ODMHSAS to provide trainings to school staff in Oklahoma. The course focuses on decreasing the stigma of mental health issues and preparing people to provide appropriate and effective assistance for someone experiencing or developing a mental health crisis.)