The trend for health care cost transparency seems to be growing as fast as health costs themselves.
HB 2216, introduced by Rep. Sean Roberts (R-Tulsa) last month, attempts to implement price transparency in the state with respect to non-contracted health providers.
HB 2216 in a nutshell
A non-contracted provider is a physician or other licensed health professional who does not have a contract with a patient’s insurance plan. This might include an out-of-network physician performing an ACL surgery or, more commonly, a non-contracted emergency physician who sees a patient with a stroke or heart attack.
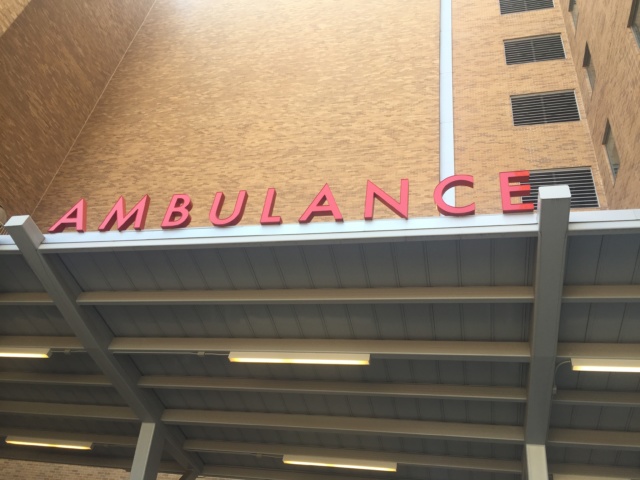
The latter situation, in particular, can lead to multiple bills from different entities — the hospital, lab, radiology and emergency physician, for instance.
Emergency departments tend to increase a patient’s exposure to non-contracted providers, not only because the need for emergency care is inherently unpredictable, but also because emergency departments host many physicians and groups who may or may not have contracts with a particular insurance plan.
HB 2216 approaches the issue of price transparency predominantly by introducing two rules for non-contracted providers:
First, non-contracted providers (presumably in non-emergency situations) are required to provide notice to patients that they do not have a contract with a patient’s insurance plan. Second, they must provide a “good-faith estimate” of charges to patients.
Also, under the bill, the time frame for these notices would be 14 days prior to rendering services in non-emergency situations and “as soon as practical” for medical emergencies.
A problem without an easy solution
While HB 2216 passed the full House on Tuesday by a 93-0 vote, whether it presents a feasible mechanism by which to increase price transparency remains in doubt.
Although a good-faith estimate might make sense when buying a house, it is impractical in medicine.
Medical costs are unpredictable. This is especially true in emergency departments, where the nature of a patient’s condition can be in flux.
Provider cost and timing of care are also relevant issues. How will the additional costs associated with generating good-faith estimates be handled? Is it worth delaying a patient’s care, particularly in non-elective situations, to undertake the time-consuming process of generating charge estimates? How will the state enforce the time lines introduced to notify patients?
Ultimately, price transparency is a complicated problem without an easy solution. While HB 2216 takes a respectable stab, it may struggle to increase patient control over pricing in practice.
Those questions and details should be discussed further when the bill begins its journey through the Senate in the coming weeks.
 Loading...
Loading...