Breastfeeding a newborn baby is the most natural thing in the world. But it can also be a difficult and frustrating experience for many new mothers, either because of problems with milk production or because infants can be mysteriously picky eaters.
This is where lactation consultants come in. And if you’ve breastfed a baby in Oklahoma City in the past 20 years, there’s a good chance you might have benefitted, at least indirectly, from the work of Becky Mannel.
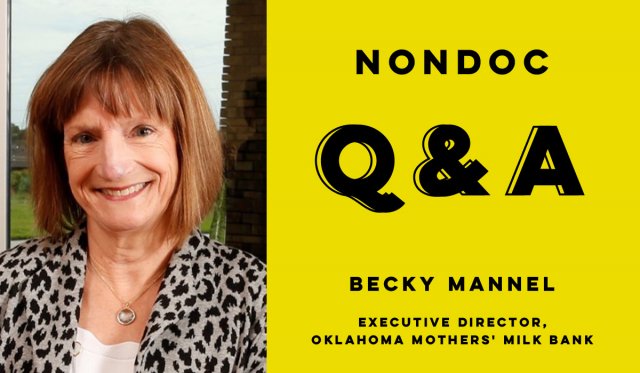
Mannel is an international board certified lactation consultant who, in 1999, started the lactation program at the OU Medical Center and Children’s Hospital and has since come to wear “multiple hats,” as she puts it, in the lactation field. Those hats include being the director of the Oklahoma Breastfeeding Resource Center, a faculty member at the OU Health Sciences Center and the current president of the Human Milk Banking Association of North America.
She is also the executive director of the Oklahoma Mothers’ Milk Bank, which distributes donated breastmilk to preterm and unhealthy babies who wouldn’t otherwise have access to the unique benefits breast milk provides.
Donated breast milk can often make a huge difference to these infants. In fact, a bill that would require Medicaid in Oklahoma to “provide Medicaid coverage for medically necessary pasteurized donor human milk” if either a mother or baby is physically or medically unable to breastfeed passed the Senate earlier this month and, as of Monday morning, is waiting to be heard by the House Appropriations and Budget Committee.
NonDoc recently interviewed Mannel about her work and the Mothers’ Milk Bank. The following exchange has been edited lightly for grammar and clarity.
You’ve worked in lactation for almost 30 years. How did you first get interested in the field? And has the science and culture surrounding breastfeeding changed a lot in that time?
As did many lactation consultants around my age, I became interested in the lactation field through my own personal experience trying to breastfeed our first child. I found that when I was struggling to nurse my son and he was losing weight, none of the physicians that we knew could help me, including my own husband, who was in OB/GYN residency!
I was often told to just quit, which I did not appreciate. How can everyone recommend breastfeeding and then not help a mother when she has problems? After weeks of struggle, frustration and formula supplementation, I learned that the hospital had hired a lactation consultant, and I immediately scheduled an appointment. With her guidance, I rebuilt my very low milk supply, returned to exclusive breastfeeding and nursed my son to 14 months.
When we moved to Oklahoma and had our third child, I had learned a lot and became the informal expert for the OB department where my husband was on faculty. I continued to expand my education and gained clinical experience until I achieved certification as an international board certified lactation consultant (IBCLC).
I am very glad to say that the science and culture around breastfeeding has changed a lot in that time. Thousands of research studies have been done in the lactation field. Breastfeeding is now a serious public health issue with federal and state attention focused on improving breastfeeding outcomes. I work closely with our state health department on several statewide initiatives to improve breastfeeding rates, including supporting the Oklahoma Mothers’ Milk Bank.
A lot of people probably haven’t heard about the Oklahoma Mothers’ Milk Bank and might never have reason to encounter it. Can you tell us about how it came to exist and why? Who benefits from the milk bank?
As an IBCLC, I started the lactation service at OU Medical Center/The Children’s Hospital in 1999. When you work with very preterm babies in a large neonatal intensive care unit (NICU), you quickly learn the research about and see the impact of exclusive human milk feedings on the survival and long-term health outcomes of these tiny humans. You see that many of their mothers have their own health complications and really struggle to provide any or enough of their own milk.
Safe, pasteurized donor human milk (PDHM) is the next best thing for these babies, and we did not have it here in Oklahoma. We would help mothers donate milk to the nearest milk bank in Texas, and I worked with our neonatologists to make the case to start providing donated milk in our hospital. We had already established a very successful milk depot to make it easy for donor mothers to drop off their milk, and we would ship it to Texas for pasteurizing. In fact, we had quickly become the largest depot for the Mothers’ Milk Bank of North Texas, which laid the groundwork for launching efforts to develop our own milk bank starting in 2011.
We acquired our nonprofit status and then spent two years fundraising. We were able to start operations in early 2013 and pass our first accreditation by the Human Milk Banking Association of North America (HMBANA). We dispensed our first batches of safe, pasteurized milk in August 2013, and we were the 13th operational milk bank in the U.S. By 2014, all Oklahoma hospitals with Level III NICUs were providing PDHM to their patients.
Readers might be surprised to learn that there’s enough unused breast milk out there to run a milk bank. Who is donating the milk? Do you usually have enough donors to meet the demand?
Most of our milk comes from healthy, breastfeeding mothers who have extra milk to give and want to help other babies in need. All donors go through a rigorous screening process, similar to blood donation screening, and have their blood drawn one time to rule out certain diseases, such as HIV. Once approved, they do the extra work of expressing and storing their milk at home just to donate to the milk bank. We work closely with our donors and really build relationships with them, especially if they donate over several months or even years. We particularly want to make sure that the donor mother, who is not paid for her milk, always has enough milk for her own baby before she ever gives any to the milk bank. We thus require a signed letter from her health care provider and her baby’s provider to verify that donating milk will not compromise the health of either the donor or her baby.
A very special group of donors are our bereaved donors, mothers who have experienced a perinatal loss, whether during pregnancy (18-20 weeks or more), at delivery or from a later infant death. Our milk bank staff, several of whom are lactation consultants, too, can work with these mothers to either suppress lactation or help them if they decide they want to express milk and donate in their child’s memory. We now have a formal bereavement program and a memorial tree to honor the memory of every single baby of a bereaved donor family.
As for meeting the demand, you would be amazed at how generous our Oklahoma families are, and we usually have plenty of milk. Being a member of HMBANA also gives us a nationwide network of nonprofit milk banks with whom to partner. Whether we are in need of a bit more milk at a busy time of year (usually the Christmas holidays!) or we have overflowing freezers and can help other milk banks, we greatly value being an HMBANA milk bank.
Tell us about the logistics of gathering, processing, and distributing the milk. Is there any part of the process that was particularly tricky to implement?
Probably the most difficult part is the initial fundraising to start a milk bank, as many philanthropic organizations are reluctant to give start-up funding. Once we overcame that hurdle, we worked with HMBANA to make sure we were following their evidence-based, ethical and internationally known standards for human milk banking. We train our staff and require some to have certain certifications in food safety practices. Our clinical coordinator is a registered dietitian and a certified lactation consultant who had experience not only in lactation but in starting a hospital nutrition service, so that was extremely beneficial to our milk bank.
Donor screening and pasteurizing are the two most critical elements in our practices. We have a physician medical director who reviews any questions related to donor screening. We pool milk from at least three different donors to equalize the composition of each batch of milk, and we monitor the pasteurizer temperatures very closely to ensure it is held at the required, narrow temperature range for human milk. This method, called the Holder method, ensures that any bacteria, viruses (including the coronavirus) or parasites are destroyed without destroying all of the immune components in human milk. We do not dispense any donated milk until cultures have shown no bacterial growth.
While there is some debate about pasteurizing human milk, and even dairy milk, most of our milk goes to medically compromised babies who cannot fight off an infection that might be acquired through contaminated milk. There has never been a documented case of an adverse reaction or infection due to donated milk from a HMBANA bank.
You’ve spoken frequently about the benefits of breast milk over formula and have been critical of the formula industry. There are some mothers who struggle to breastfeed, for one reason or another, and that can be associated with a lot of shame and guilt. What would you say to a person in that situation?
I say several things, and I say this in trainings all over Oklahoma:
- We, the public health and health care communities, strongly encourage breastfeeding for the best health outcomes for parents and babies, and then we make it incredibly difficult for many to succeed at it. We can and we must do better to help mothers reach their own breastfeeding goals. Most mothers quit breastfeeding before they intended to, no matter how hard they tried. There is no shame or guilt in doing the best you can. There is and should be anger that we failed to provide timely support, whether in the hospital or after going home with a new baby. Mothers blame themselves when breastfeeding does not work out as they thought it would when we, as a society, are really the ones to blame.
- Formula itself is not an evil substance. We need good, safe, quality formulas. And we need to support breastfeeding so we can reduce the need for formula as much as possible. The formula industry, however, profits when breastfeeding does not work out, and that is a global problem. No company profits financially when breastfeeding succeeds.
- If a mother thinks her baby is not feeding well and she cannot get timely, skilled lactation support, then she needs to make sure her baby gets fed in the safest way possible, whether it’s her own expressed milk, donor milk or formula. Mothers will do what they think is best for their baby and themselves, and I absolutely support that.
- We need paid maternity leave so all parents have time to recover from childbirth, bond with their new baby and establish breastfeeding. European countries that have federal policies for paid maternity leave have huge decreases in their infant mortality rates.
Every once in a while, there’s an off-beat news story involving breast milk — for instance that it’s a fad among bodybuilders, or that it’s being used to make ice cream. And if you go on Craigslist, you can always find a couple of ads from people selling breast milk. What’s your reaction to these stories? And do you ever get calls from people wanting milk for these alternative purposes?
These kinds of stories either sadden or infuriate me. When we take the special relationship of a mother nursing her baby, the unique qualities of human milk that promote optimal growth and development and protect from infection (including COVID-19), and we commoditize human milk into something to sell and profit from, we are exploiting women and women’s bodies.
I want people to hear the real stories. The calls we get are the calls from mothers diagnosed with cancer who have to stop breastfeeding because of cancer treatments and are desperate to get safe, donated milk for their babies. The foster parent whose baby cannot tolerate any type of formula, is diagnosed with failure to thrive, and Medicaid will not cover the cost of donated milk from the milk bank, so our milk bank works with DHS to cover the cost together. The bereaved mothers, at a time of terrible loss, who go out of their way to pump and donate milk to honor the baby they lost by helping other babies.
Our milk bank team goes out of its way to help every single parent who calls, in any way we possibly can. We connect them with local resources, such as our Oklahoma Breastfeeding Hotline, if a mother needs help to increase her milk supply or has other breastfeeding difficulties. We advocate for change by educating health care providers, students, hospital staff and community health departments on the importance of breastfeeding and donor milk. And we are currently working with the Oklahoma Legislature to pass a bill to require Medicaid to cover safe, pasteurized donor human milk from HMBANA banks for babies in a home setting with a medical need. SB 469 passed overwhelmingly in the Oklahoma Senate and is in the possession of the Oklahoma House. Please help us to get it passed!