Amid a pandemic that has created staffing shortfalls, Emergency Medical Services Authority, the entity that provides emergency medical transport services in Oklahoma City, struggled to meet its required response times in 2021.
Under its current agreement with Oklahoma City, EMSA is required to respond to Priority 1 calls in less than 11 minutes, at least 90 percent of the time. It must respond to Priority 2 calls in less than 25 minutes, at least 90 percent of the time.
Priority 1 calls are those that can include life-threatening situations like heart attacks, strokes and serious injuries sustained in car accidents.
Priority 2 calls are less severe and include falls, broken limbs and minor vehicle accidents.
EMSA is a public trust authority that was established in 1977 by Oklahoma City and Tulsa to provide ambulance services in the two cities. The authority is overseen by an 11-member board of trustees, eight of whom are appointed by the mayors of OKC and Tulsa.
EMSA is currently the state’s largest provider of emergency medical care outside a hospital setting, according to its website. As a public trust, EMSA is tasked with overseeing emergency response in its service areas, including contracts with private ambulance companies and other entities.
In 2013, EMSA contracted with the company American Medical Response for ambulance services, in a deal that included a two-minute increase in required response times. The contract with AMR was terminated in October 2020 as a result of “multiple contractual defaults by AMR,” and EMSA has since been managing operations directly.
On Jan. 18, Jim Winham resigned as president and CEO of EMSA and chief compliance, and administrative officer Johna Easley stepped into the role on an interim basis.
That’s not the only legal dispute EMSA or its employees have faced. Winham had succeeded longtime president H. Stephen Williamson, who resigned in 2017 after 39 years leading EMSA. Williamson was the subject of a federal lawsuit alleging he accepted illegal kickbacks from former EMSA contractor Paramedics Plus. Williamson denied the allegations, and the case was eventually settled. He died in 2018.
The OKC City Council decided in October 2021 to hold off on renewing its agreement with EMSA and is now in a six-month evaluation period to decide the future of the city’s relationship with the public trust. If the relationship with EMSA is terminated, it is unclear what the next move would be for the city’s ambulance services, although they could end up under the purview of the Oklahoma City Fire Department.
EMSA response times lagging
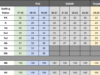
EMSA’s response times for Priority 1 calls grew longer in Oklahoma City in 2021.
The latest data on the EMSA website, which goes through December 2021, shows an organization struggling mightily to reach its 90-percent on-time requirement in the OKC area.
It started the year at 68 percent and ended the year at 52 percent. Although the rate rose in some months, it never got higher than 76 percent.
EMSA spokesman Adam Paluka said the organization has faced staffing issues throughout the pandemic.
“EMS staffing is a complex situation, and EMSA is not immune to staffing issues EMS providers across the country confront each day,” Paluka said. “Right now, we have 11 medics out with COVID and potential COVID exposures in our Western Division (in the OKC area). We are also dealing with hospital bed delays, increased call volume, and medics who have worked through a 22-month-long pandemic. All of that affects staffing and response times.”
OKC deputy city attorney Wiley Williams, who is also a city representative on EMSA’s board of trustees, said many of the delays are the result of EMTs and Paramedics being required to stay with patients until they are admitted to the hospital. Hospital crowding owing to COVID-19 has contributed to longer admission wait times.
“When EMSA picks up a patient and takes them to the hospital, they can’t abandon the patient until they’re admitted or moved to a room,” Williams said. “So if there’s no beds at the inn, they have to stay with that patient, and sometimes that can be for two, three, four, five hours at a time, and at multiple hospitals. It happens regularly.”
Oklahoma City’s vast municipal acreage also poses an obstacle. Though ambulances are stationed all around the city at any given time, coverage gaps have become common.
“Oklahoma City by itself is about 500,000 or 600,000 people and is 620 square miles,” said Justin Hunter, the director of the paramedicine program at Oklahoma State University OKC. “It’s one of the top two or three biggest cities as far as square miles in the country. When you have a city that is so spread out, there are some unique challenges.”
Follow @NonDocMedia on:
Ordinance change could help ease staffing problems
Oklahoma City and Tulsa recently took steps to improve EMSA’s response times and ease personnel strains.
In November, the OKC City Council approved a request by EMSA to allow some ambulances in the fleet to be classified as Basic Life Support (BLS) rather than Advanced Life Support (ALS). The change allows BLS ambulances to be staffed only by emergency medical technicians (EMTs), rather than by paramedics, who have a higher level of training.
“What separates EMTs and paramedics in terms of education is an advanced skill set as far as what kinds of procedures they can perform and what types of medications they can give,” Hunter said. “That’s far more broad as a paramedic.”
Curtis Knowles, EMSA medical director, said in a November City Council meeting that the change would improve efficiency.
“Historically, Oklahoma City has received an all-ALS service, meaning there is a paramedic on every ambulance,” Knowles said. “The benefit to that is when they arrive they have the highest care available to perform procedures. But it does create a situation where we have over-triage. Very often, you go and there is a parking lot car accident, or someone who stubbed their toe three weeks ago and they want an ambulance to take them to the hospital. So the paramedics aren’t being utilized to the fullest capacity on all calls.”
Hunter, who also works for EMSTAT, which provides ambulance service in Norman, agreed. He said the tiered system is common in large municipalities and is a good approach.
“From my point of view, with lower-acuity calls it will improve efficiency,” he said. “It’s important to get the appropriate level of care to each call. If you go to the ER, they don’t give everyone a CT scan.”
Meeting the demand for paramedics and EMTs

Although meeting current staffing needs appears critical, a larger issue involves making sure emergency-service providers such as EMSA are able to hire qualified and well-trained staff in the long-term.
Many of central Oklahoma’s paramedics and EMTs are trained through the OSU-OKC paramedicine program Hunter oversees, and he said demand for graduates has never been higher.
“It’s been a very quick turning of the tables,” Hunter said. “Over the last 30 years, across the country there was less demand and a high supply, and it wasn’t easy to get certain jobs. But the demand for paramedics has gone through the roof.”
Hunter said the coronavirus pandemic has driven some of the demand, along with other factors, such as experienced paramedics moving into hospital settings.
“The supply of paramedics has shriveled up, and now we’re starting to see pay skyrocketing and massive demand everywhere,” he said. “It’s not a local thing. It’s everywhere.”
EMSA’s efforts to hire qualified candidates remain ongoing and challenging.
“We are working tirelessly to recruit medics to EMSA,” Paluka said. “We have stepped up our out-of-state recruiting efforts, developed a recruiting website joinemsa.com, and have started to build a ‘Earn While You Learn’ program to help qualified applicants go to EMT school while earning a paycheck. That is one way we will grow our EMT ranks.”
Hunter said paramedic and EMT students tend to be young, between the ages of 22 and 35, although he recently had a 66-year-old pastor in his program.
“Typically, they’re people who like to help other people,” Hunter said. “They’ll stop to help change a flat tire or chase someone down who has stolen an old lady’s purse. They want to put themselves in a position to help, and for a lot of people that EMT program is the exposure that creates a gateway to go into becoming a paramedic.”
The window of opportunity
The city’s contract with EMSA comes up for renewal every five years — most recently in October 2021 — and the review period lasts for six months, ending in April.
“When the city merged to create this trust, they provided in the trust document itself a period of every five years in October to exercise the right to get out of the contract with a year to settle up everything,” Williams explained.
This periodic option to renew is known as the “window of opportunity.” During that time, city officials will continue to evaluate EMSA’s response times to calls as well as its ability to maintain staffing levels for its ambulances amid the pandemic.
“2021 was that year for the window of opportunity, but because of the situation with COVID, the city manager (Craig Freeman) wanted to take another look in a few months to see how that is going to play out, so he asked for an extension through April,” Williams said.
If Oklahoma City were to opt out of its relationship with EMSA, the Oklahoma City Fire Department would likely take over ambulance services in Oklahoma City. It’s not clear how much that would improve response times. The department does have numerous paramedics in its ranks and already responds to most medical calls, but it does not transport patients.
“The city manager and the Council will evaluate whether they stay in the (EMSA) system or take on the problems themselves,” Williams said. “The issues aren’t going away overnight, and I think the city manager recognizes that. Whatever they decide ultimately will be a council decision, and we’ll deal with that at the time. OKC is in a better position to get out of the system than Tulsa is, because we’ve been buying our own equipment.”
Ward 6 Councilwoman JoBeth Hamon said that, based on what has been presented in meetings, the wait times are the central issue being looked at during the six month window.
“From what I understand, that was the tipping point for not doing a blanket renewal and going through this review process,” she said. “What they shared with us was the wait times were something that needed to sort of be re-evaluated.”