The numbers tell the story.
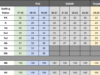
According to a report released in January by the National Institute on Drug Abuse, the U.S. crossed a gruesome milestone in 2021: 100,000 people died of drug overdoses in just one year. Not only is this the highest number of overdose deaths in our country’s history, but the trajectory shows these numbers climbing every month.
Some have called the overdose crisis a “lost epidemic within the pandemic.” And, in ways, it has outpaced COVID-19. In 2020 and 2021, more than 57,000 Americans between the ages of 18 and 49 died of COVID-19, according to data from the CDC. Comparatively, during approximately the same period, nearly 79,000 people between 18 and 45 died of fentanyl overdoses alone, according to data analysis from the organization Families Against Fentanyl. In fact, fentanyl overdoses have become the leading cause of death for adults between the ages of 18 and 45 in this country.
Yet, while this tragedy surges, our society has failed to implement effective measures to combat it. According to the same report cited earlier from the National Institute of Drug Abuse, in 2020 only 13 percent of people with drug use disorders received any treatment at all.
Immediate and aggressive action is required, centered on both prevention and treatment. The good news is that there is plenty of evidence telling us how to get started, and one of the first steps is tearing down the barriers that keep people from getting help.
Barrier 1: Addiction is a chronic disease
It is important that we eradicate the view of addiction as the result of moral failing, lack of willpower, or an unwillingness to stop. Addiction is a chronic disease that shares many features with other chronic illnesses, including heritability, an onset and course influenced by both environmental and behavioral factors and, most importantly, the ability to respond to appropriate treatment.
Like chronic conditions such as diabetes or cardiovascular disease, addiction is treatable, often in ways that include long-term lifestyle modifications. Viewing addiction care through the lens of chronic-disease management instead of repeated episodic treatment is a sustainable, evidence-based model that shows real promise.
However, many people don’t seek addiction treatment for reasons directly related to stigma resulting from a failure to view addiction as the health condition it is; they are simply ashamed of their disease. Changing this approach is paramount to getting people into treatment.
Barrier 2: Access to treatment
Addiction crosses all geographic, demographic and sociological borders, but access to health care does not.
Also, addiction is not a nine-to-five disease, though traditional treatment resources often function as such. The current best-practice treatment plan for addiction calls for an approach that works within a recovering addict’s life, rather than becoming their life. It is important to allow those seeking recovery to access help where and when they need it.
RELATED
How to find a therapist in Oklahoma by Jeanette Moore
Ideally, we would provide access to treatment at the initial sign of crisis and then provide continuing care for an extended period of years (not months). This approach not only leads to better health outcomes but also saves countless dollars on medical care, judicial complications, workforce shortages and a host of other expenses associated with untreated drug abuse and misuse.
If there has been one positive outcome from the COVID-19 pandemic, it is increased access to, and comfort with, digital medical platforms, both among patients and behavioral health providers, who have previously been slow to adopt the technology.
These platforms can bring addiction care to people who might not otherwise have the ability to seek it out. Via telemedicine, individuals in treatment can have 24/7 access to professional care from clinicians and counselors.
Having immediate access to a licensed professional counselor has proven to lead to better outcomes for people in the throes of crisis or on the verge of relapse. The process of digital access also allows caretakers to gather and analyze data that can, in turn, lead to better overall mental health outcomes.
Barrier 3: Incarceration is not the answer
Studies have shown that moving away from punitive responses to nonviolent drug offenses not only leads to better outcomes for the individuals impacted but provides relief to an expensive and overburdened prison system.
Jail diversion programs, which send people to rehabilitation programs instead of incarcerating them, are not a new concept, but they have been gaining popularity in recent years. People sent to these programs have higher recovery rates and lower re-offense rates than those sent to jail. Such programs ensure addicted individuals receive treatment they might not get otherwise and offer budgetary savings without increasing the risk to public safety.
The time to take action is now
In 2020, the Oklahoma Department of Mental Health and Substance Abuse Services launched a five-year strategic plan that lists reducing overall substance abuse in the state as one of its three main goals. Achieving this goal will require breaking down these barriers to treatment and focusing on long-term mental health outcomes.
This will require a shift in how we think about and approach addiction itself. The bottom line is that there is not one easy fix to the drug epidemic facing our nation and our state. The complexities of tackling the issue require out-of-the-box thinking, strategic public-private partnerships and an assertive approach that relies on education, state-of-the-art technologies and an overall change in mindset.
It’s a tall order, but it’s an absolutely necessary one.