When COVID-19 hit Oklahoma this spring, public health officials scrambled to ramp up the state’s contact tracing operations. But the scale of the pandemic has put a strain on capabilities, with outdated technology and a sometimes uncooperative public making it difficult to keep up with a process in which speed and thoroughness are key. As a result, Oklahoma’s top public health officer now says the state needs to rework its contact tracing system.
“We’re looking at contact tracing in the future and basically how to redesign it,” Oklahoma State Health Commissioner Dr. Lance Frye told NonDoc on Nov. 19. “Because I think it probably does need to be redesigned. I don’t think that when the pandemic first started and they said everybody start doing contact tracing and the old-fashioned public health and epidemiology stuff — that was not really designed for a pandemic.”
According to Aaron Wendelboe, an epidemiology professor at OU who served as the interim state epidemiologist from March through the beginning of August, a failure to implement effective contact tracing has played a role in the record numbers being seen now in Oklahoma and across the country.
“If we’d ever been able to get on top of the contact tracing, I think that we would have had a much better chance. But, as you know, it wasn’t just Oklahoma. Essentially nobody in the states has done really a great job of contact tracing,” Wendelboe said, comparing the U.S. to countries such as South Korea and Taiwan, where contact tracing has helped to contain the virus.
But as things now stand, Oklahoma’s public health infrastructure is stretching to keep up with the surge in cases, modifying some tracing procedures and letting some cases go untraced because the health departments can’t investigate them quickly enough.
Early contact tracing obstacles
Like many places in the U.S., Oklahoma encountered a number of hurdles as it scrambled to begin contact tracing for COVID-19.
“Over all, I’m proud of what we were able to accomplish, because we were building something while also trying to do it,” said Wendelboe, who helped formulate Oklahoma’s response at the time.
But he also described a number of challenges that prevented the state from doing early, effective contact tracing, including hiring and training staff, finding a space to serve as a call center and establishing lines of communication both within the OSDH contact tracing team and between the state’s many county health departments.
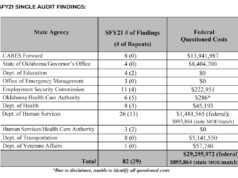
Throughout the COVID-19 pandemic, Oklahoma’s response has been hampered by outdated technology. Computer glitches and other system failures initially caused delays in daily infection reports and led to huge backlogs in unemployment claims. The deficient technology presented many hurdles to effective contact tracing.
“We know the technology is there,” Wendelboe said. “But when it came to reporting of disease and contact tracing, we were at least 20 if not 30 years behind.”
For instance, the state’s disease-surveillance system, Public Health Investigation and Disease Detection of Oklahoma (PHIDDO), could not communicate with the MTX/Google contact tracing system the State Health Department was trying to use or with the call-center software inContact. It also didn’t have the tools needed to do things like hand over cases between shifts or track multiple locations as potential sites for transmission.
“The PHIDDO system is old,” Wendelboe said. “It wasn’t easily customizable. It would crash on a regular basis.”
Frye announced in September that the state would be moving its COVID-19 reporting entirely off the PHIDDO system and onto the MTX/Google system.
But early on, tests were getting sent to a number of different laboratories, which used a variety of different protocols for reporting the results. Wendelboe explained that this meant State Health Department employees would often have to follow up with labs to standardize the information collected for each individual case before contact tracing could even begin.
The fix for some of these problems came from the federal level, Wendelboe said. The U.S. Department of Health and Human Services standardized the reporting format and the CDC provided IT support.
New challenges as numbers surge
The system is working somewhat better now. According to Lee Anne Bruce-Boone, the chief for the Office of Accountability Services, who has been heavily involved in setting up contact tracing, OSDH now has approximately 400 employees doing case investigation and contact tracing. They work in coordination with about 150 employees working out of county health departments, with the exception of Tulsa and Oklahoma Counties, which are running independent tracing operations.
The state has also started using the MTX/Google tracing system to automate parts of the tracing process, which speeds things up considerably, though the initial follow-up with each confirmed positive case is still done by phone and can take from 30 minutes to an hour to complete.
With daily case numbers now in the thousands, Bruce-Boone said things are “definitely busy,” and the department has made some modifications to its procedures to keep up with the numbers. For instance, investigators used to make six attempts to contact people who tested positive, but now they try only four times, Bruce-Boone said.
Bruce-Boone said people not responding to contact attempts is currently the major hurdle to tracing. Many people don’t answer the phone. Others don’t want to give out information about their contacts.
Anthony Triana, a spokesman for Saxum, a public-relations firm contracted by OSDH, said that because of the transfer from PHIDDO to MTX, the state is not currently able to provide a complete numerical picture of the data from both systems. So it’s not entirely clear how many cases are not going through the contact-tracing process.
“We have contracted with a data analytics team to extract data from both systems and examine in-depth, but this process is in its infancy and results will likely not be available for some time,” Triana wrote.
The data from PHIDDO alone, however, show that approximately 10 percent of cases in October were lost to lack of response.
Anecdotally, the numbers seem like they might be higher. Bruce-Boone said about a third of people answer on the first attempt. Wendelboe said he’d heard that anywhere from 40-60 percent of those contacted either don’t respond or don’t want to cooperate.
Oklahoma County experiences additional delays
In Oklahoma County, contact tracing for COVID-positive patients can take days or weeks, if it even happens at all.
Hieremila Haile, the Oklahoma City-County Health Department’s chief epidemiologist, said that while improved technology has helped, lingering technological issues are still affecting the county’s contact tracing operation.
“There is a delay in reporting,” Haile said. “Say you go get tested today. Oftentimes your doctor will tell you pretty soon after that you’re positive. When you get that notification, that doesn’t mean we’ll get that notification at the same time. Oftentimes it takes some time for the lab to then report that to the state, and then it comes down to us. And that span can be a couple of days or even up to a week.”
For COVID-19, which has an average incubation period of five days, it’s important to get to people who have been exposed fast. The effectiveness of contact tracing reduces significantly each day the process is delayed, particularly if it’s been more than a week since system onset.
Haile said her department often doesn’t follow up on cases that they receive more than a week after the fact. Between delays and people not responding to calls during one week in November when cases were spiking, the department was able to initiate the tracing process with only about 70 percent of people within a week of infection, Haile said.
During the summer, when the state was having problems with reporting backlogs owing to tech issues, the county would often receive test results weeks late, she said.
Wendelboe commented that while epidemiologically contact tracing becomes futile at a certain point, not following up on cases can present its own problems.
“We need to maintain the trust of the public,” he said. “I think when people who get sick don’t ever get a call from the health department, I think that they feel like public health is failing them. (…) So we have this dichotomy. We have half the population who won’t take the phone call, and then we have half the population that gets upset if they don’t get a phone call.”