
Amid an air of confusion over its own powers and responsibilities, the Oklahoma Health Care Authority Board voted this morning to authorize financial expenditures for contracting with managed care organizations, controversial entities that take a portion of public Medicaid funding for attempting to improve care coordination, increase patient compliance and decrease overall program costs.
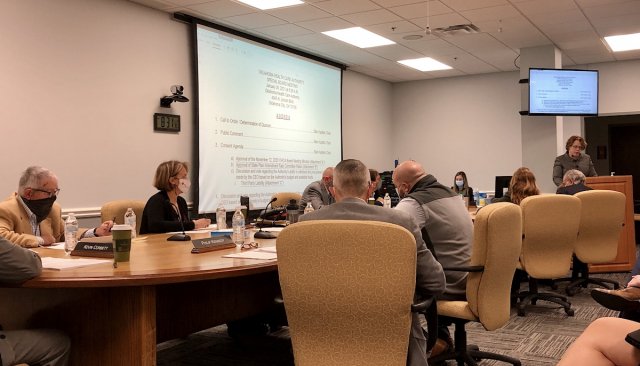
Companies responded in December to the OHCA’s requests for proposals regarding third-party managed care. Gov. Kevin Stitt’s pursuit of implementing managed Medicaid contracts has been opposed by many state legislators and health professional associations. As a result, some OHCA board members attempted unsuccessfully to table and reject the funding authorization votes during Tuesday’s meeting.
“The reality is, the urgency for this matter and the health outcomes of the state have been lingering for decades,” OHCA CEO Kevin Corbett said. “I don’t know why we would want to wait when we have a plan and we have a process to move forward with this.”
Board members debated whether they have the authority to approve a managed care contract after the Oklahoma Legislature reformed the agency’s governance in 2019. That reform authorized Stitt to hire Corbett directly, and the governor holds appointment authority for five of the nine board members.
“This is not unusual to vote on a budget item like this at this point in the budget process,” said board member Marc Nuttle, who voted in favor of the managed care organization RFPs.
‘The math simply does not add up’
Before the board took its action Tuesday, five representatives of major health care associations offered public comment asking members to oppose the managed care effort. Several referenced Oklahoma’s past managed Medicaid effort from the 1990s, which was ended owing to many of the same concerns opponents are voicing now.
“We urge you to closely examine why legislators currently oppose the [managed care model],” said Debra Billingsley, director of the Oklahoma Pharmacists Association. “The Oklahoma Pharmacists Association is not supportive of bringing in managed care because managed care organizations are motivated by profits and are linked to pharmacy benefit managers.”
Lynn Means, the Oklahoma Dental Association’s director, said the 1,000 dentists who accept SoonerCare — as Oklahoma’s Medicaid program is called — “stand unified” in their opposition to returning to third-party managed care. She said about 90 percent of Medicaid-accepting dentists stopped accepting SoonerCare when Oklahoma used third-party managed care companies in the past.
“As a reminder, dental Medicaid is only available to children in Oklahoma,” Means said. “How can sending our tax dollars to an out-of-state private insurance company that operates with significantly higher administrative costs save money while maintaining the same level of care and the same number of dentists who provide that care? The math simply does not add up.”
OHCA staff are evaluating the proposals from managed care organizations and are expected to make their selections before the end of the fiscal year June 30. The amount of Medicaid funding that could be managed by the organizations tops $2 billion.
It is possible that members of the Oklahoma Legislature could attempt to pass statute during the 2021 session, which starts Feb. 1, that would prevent implementation of Medicaid managed care.




















